Blood pressure needs to be maintained in a narrow, healthy range for the body to function well. Regulation of blood pressure can be short-term or long-term. Short-term regulation occurs over the span of seconds to minutes and is mediated through the reflex activity of various receptors; long-term regulation occurs over the span of days to weeks and is mediated through the modulation of fluid and blood volume in the body.
Effect of autonomic nervous system on blood pressure
The autonomic nervous system comprises of the sympathetic and parasympathetic components.
The sympathetic system supplies the following:
- Arteries and arterioles
- Veins
- Directly the heart
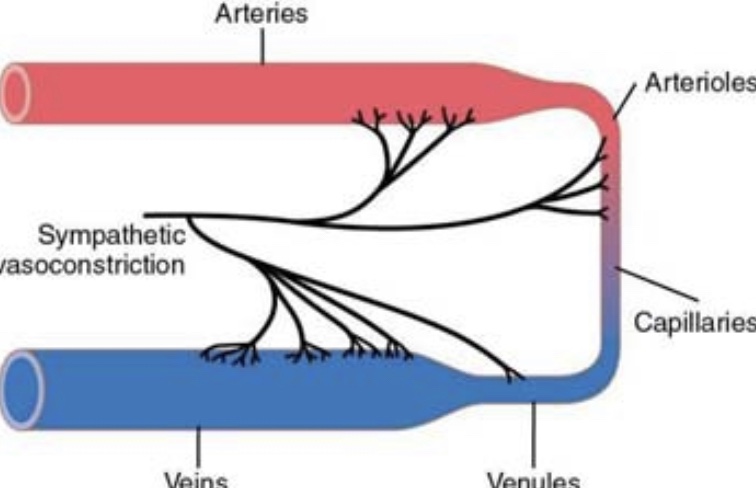
Sympathetic stimulation of the arteries and arterioles increases peripheral resistance. Sympathetic stimulation of the veins constricts them, thus squeezing extra blood into the circulation (as veins are the reservoirs of blood). Sympathetic nerves also directly innervate the heart. Upon sympathetic stimulation, the heart contracts more forcefully. Hence, due to all these effects, sympathetic stimulation acts to increase blood pressure.
The parasympathetic system is not as important as the sympathetic system when it comes to the regulation of blood pressure, but its stimulation reduces heart rate and heart contractility to some extent.
Various mechanisms of short-term blood pressure regulation
- Baroreceptor reflexes
- Chemoreceptor reflexes
- Atrial and pulmonary artery reflexes
- CNS ischemic response
Baroreceptor reflexes
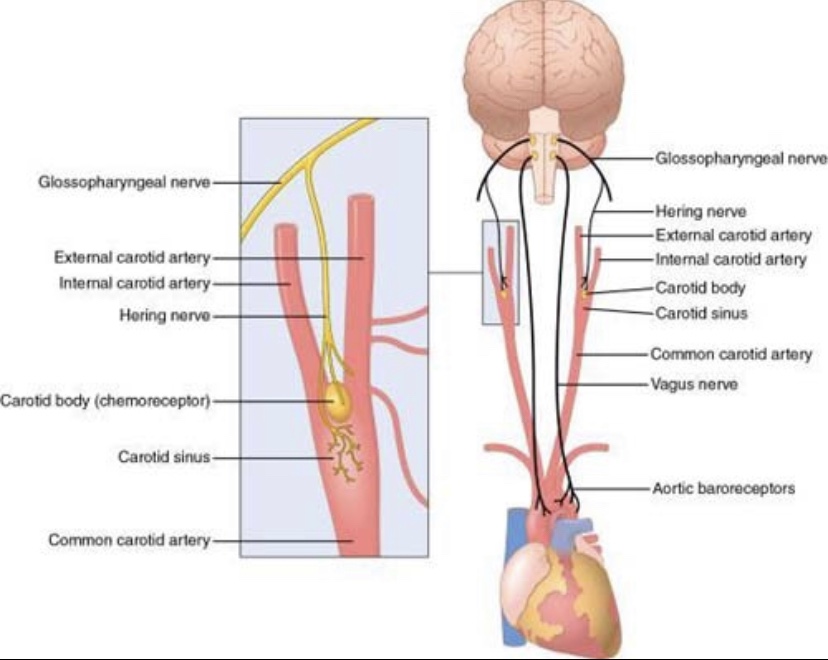
Baroreceptors are stretch receptors, located mainly in the carotid sinus and aorta, which detect arterial pressure changes. Signals from the carotid baroreceptors transmit through the glossopharyngeal nerve, while signals from the aortic baroreceptors transmit through the vagus nerve. Both of them lead up to the nucleus tractus solitarius in the medulla.
Baroreceptors are most sensitive to arterial pressure changes in the normal range, and they respond much more to a rapidly changing pressure than stationary pressure.
When blood pressure increases, baroreceptors are activated leading to the release of the excitatory neurotransmitter, glutamate. The signals reach the nucleus tractus solitarius, which stimulates both the nucleus ambiguous and caudal ventrolateral medulla. Stimulation of the nucleus ambiguous leads to the activation of the parasympathetic system. And stimulation of the caudal ventrolateral medulla inhibits the rostral ventrolateral medulla through the inhibitory neurotransmitter, GABA, leading to inhibition of the sympathetic system. These lead to the consequent lowering of blood pressure.
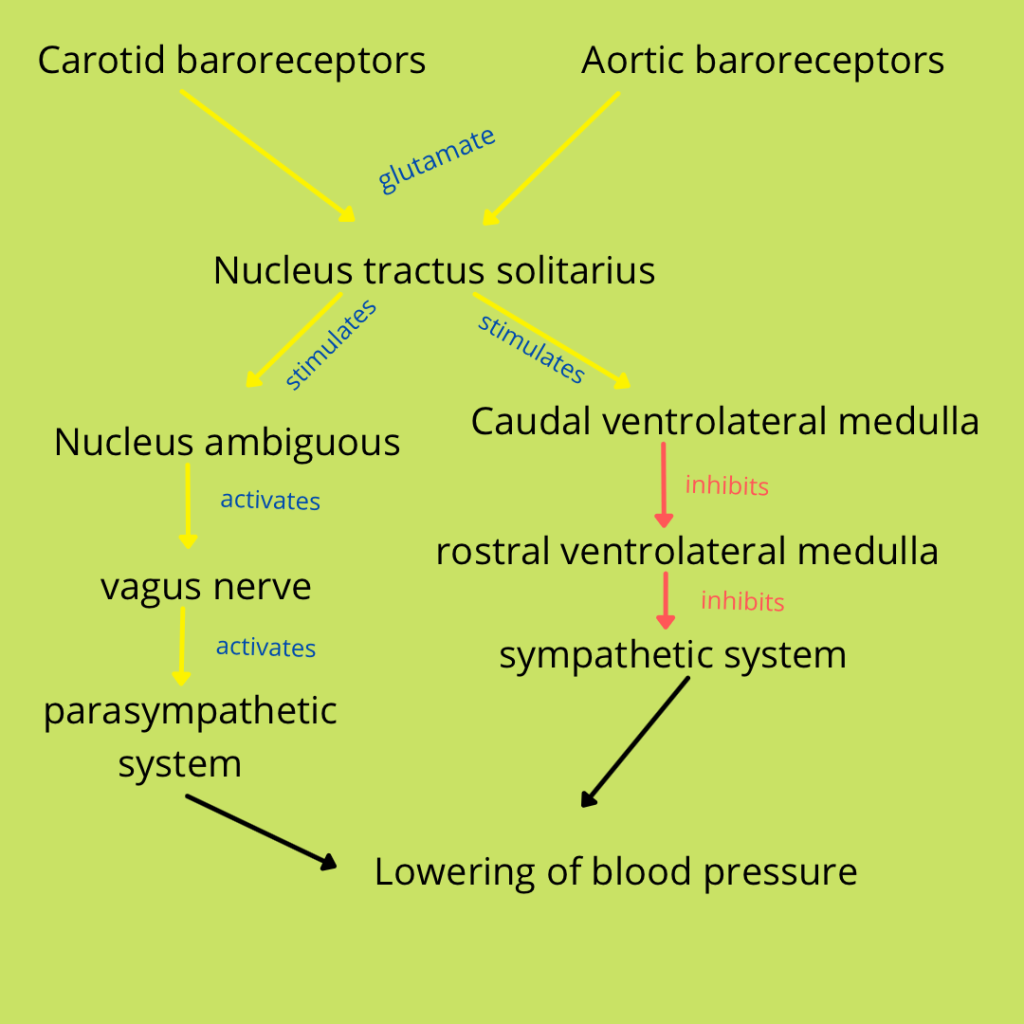
Just like activation of baroreceptors, in response to high blood pressure, leads to changes that eventually reduce blood pressure, in response to low blood pressure, baroreceptors get inhibited – hence sympathetic system is stimulated and parasympathetic inhibited – and blood pressure is increased back to normal. Thus, baroreceptors help maintain the blood pressure in the normal range.
Chemoreceptor reflexes
The chemoreceptors, located in around the bifurcation of the common carotid artery and and the aorta, primarily sense oxygen, carbon dioxide and hydrogen ion levels in the blood, but also detect very low blood pressure levels. They lead up to the vasomotor centre of the brainstem and, through subsequent knock-on effects, raise the blood pressure to normal.
Atrial and pulmonary artery reflexes
Both the atria and pulmonary arteries have low-pressure receptors in their walls. These keep the blood pressure down in the face of increase in blood volume like during sudden rapid infusion of intravenous fluids.
CNS ischemic responses
When blood flow to the vasomotor center in the lower brainstem becomes severely low, the vasoconstrictor and cardioaccelerator neurons in the vasomotor center become strongly excited, probably due to the accumulation of waste products like lactic acid, acidic substances and carbon dioxide. This is followed by very intense sympathetic stimulation – so intense that the renal arterioles get constricted, and no urine is formed. However for the CNS ischemic response to occur, the blood pressure needs to be dangerously low (below 60 mm Hg). Hence, the powerful CNS ischemic response is an emergency mechanism, not a regular one.
Other factors affecting blood pressure
Exercise and respiration also affect blood pressure. During exercise, muscular compression leads to translocation of blood from the peripheral vessels into the heart and lungs, thus leading to increase in cardiac output and arterial blood pressure. Also, blood pressure fluctuates with the cycles of respiration, more so in deep respiration. The explanation is that many of the ‘breathing signals’ that arise in the respiratory centre in the medulla ‘spill over’ to the adjacent vasomotor centre. In addition to that, during respiration, pressure in the thoracic cavity changes which contracts or dilates the blood vessels. Overall, the net effect of respiration on blood pressure is that during the early part of expiration, the blood pressure increases and decreases in the remainder of the respiratory cycle.
Leave a comment