Fetal blood circulation is different from that of adults. The lungs, which are responsible for the gaseous exchange in blood (retaining oxygen and washing out carbon dioxide) become active only after birth. So, till the time we spend in our mothers’ wombs, it is the placenta, which carries out the vital task of oxygenating and deoxygenating our blood.
The Unique Fetal Circulation
Oxygenated blood from placenta flows in through the umbilical vein, bypasses the liver, continues through the ductus venosus into the right atrium and instead of going to the right ventricle, goes through the foramen ovale (a gap between the right and left atria) into the left atrium, and then pumped by the left ventricle. The blood entering the right atrium from the superior vena cava flows to the right ventricle through the tricuspid valve. This blood is mainly deoxygenated, coming from the head portion of the fetus, and is pumped by the right ventricle to the pulmonary artery. It is then directed through the ductus arteriosus into the descending aorta, from which it is finally led to the placenta through the two umbilical arteries.
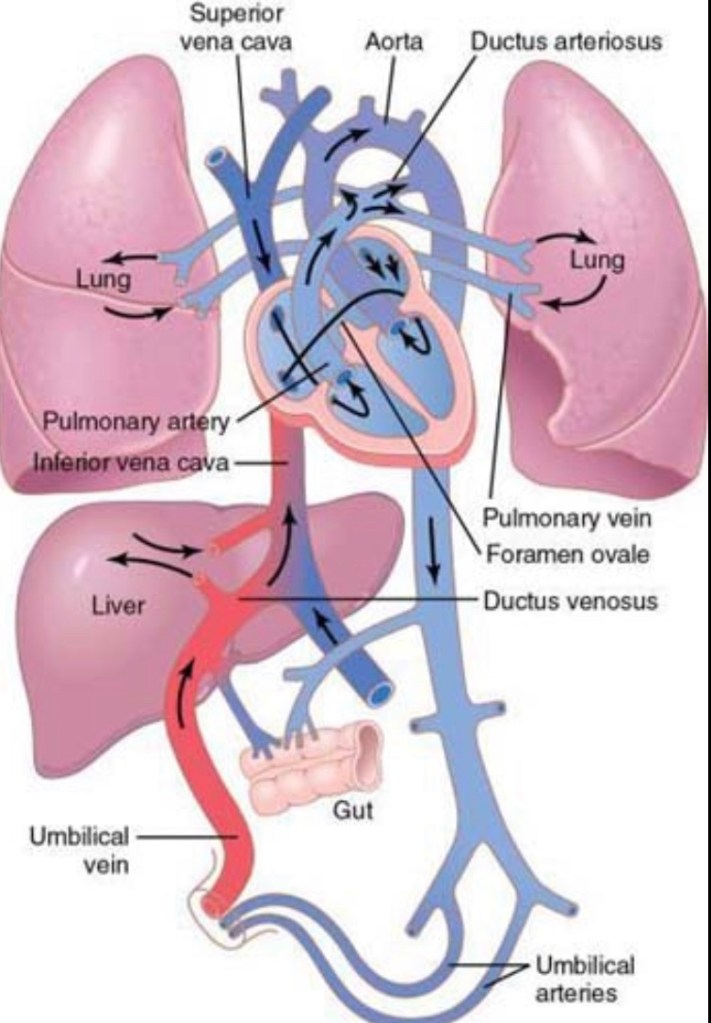
Out of the total blood flowing through the fetus, approximately 55 percent goes through the placenta; the remaining 45 percent passes through the tissues of the fetus, out of which only 12 percent passes through the lungs.
Changes in circulation at birth
Decreased pulmonary and increased systemic vascular resistances
As blood flow to the placenta ceases after birth, the systemic vascular resistance increases immensely, which in turn increases the pressure in the aorta, left ventricle and left atrium. Also, the pulmonary vascular resistance greatly decreases due to the expansion of the lungs. This occurs due to opening of the lung vessels and oxygenation of the lung tissue.
Closure of foramen ovale
The foramen ovale closes due to the low right atrial pressure and high left atrial pressure, which occur secondarily due to the changes in systemic and pulmonary resistances at birth. Functional closure of the foramen ovale happens immediately after birth; anatomical closure takes weeks, and in some, it may never happen. Still, blood doesn’t flow from the right to left atrium due to their pressure differences. Also, blood doesn’t flow from the left to right atrium, as this would close the flap on the foramen ovale.
Closure of ductus arteriosus
Due to the circulatory changes at birth, blood might tend to flow from the high pressure aorta to the pulmonary artery through the ductus arteriosus. However, the ductus arteriosus closes due to increased oxygenation and decreased prostaglandin secretions. Hence in premature infants, a prostaglandin inhibitor, indomethacin, can lead to closure of the ductus arteriosus.
Closure of ductus venosus
The reason behind the closure of the ductus venosus is not very clear, but within 1-3 hours of birth, the ductus venosus contracts strongly, which raises the portal venous pressure, and blood starts flowing through the liver.
Some features of neonatal circulation
Blood volume
Neonates have an average blood volume of 300 ml after birth. However, if the placenta is left attached to the neonate for a few minutes after birth, around 75 ml extra blood is squeezed into the neonatal circulation. This extra blood volume is beneficial but may cause pulmonary edema with mild respiratory distress.
Cardiac output
The cardiac output of a neonate averages around 500 ml per minute.
Arterial pressure
The arterial pressure during the first day of birth is around 70 mmHg systolic and 50 mmHg diastolic and increases gradually over the next several months to about 90/60 mmHg.
Congenital heart defects
They can be of three types:
- Stenosis of the heart vessels
- A left-to-right shunt: an anomaly in which blood flows from the left to right side of the heart
- A right-to-left shunt: an anomaly in which blood flows from the right to left side of the heart
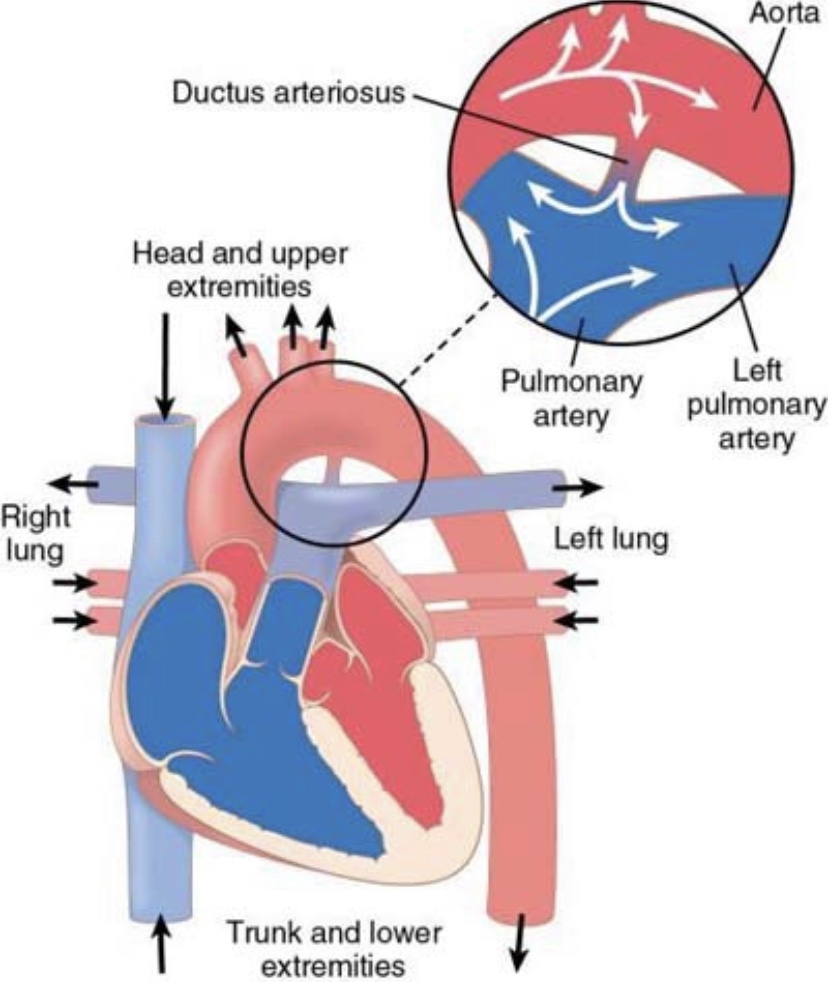
Patent ductus arteriosus
In about 1 in 5500 babies, the ductus arteriosus persists, and this results in a left-to-right shunt. Oxygenated blood from the aorta reflows through the patent ductus arteriosus into the pulmonary artery and hence lungs. In the early months of an infant’s life, a patent ductus arteriosus doesn’t cause much problems. But, as the child grows, the gradient between the high pressure in the aorta and low pulmonary artery pressure increases, thus causing problems. In particular, the cardiac and respiratory reserve diminish. The heart is already stressed from doing a lot of work and can’t work harder during exercise. Also, the lungs may get congested with fluid; so they don’t work optimally either. Clinically, a murmur might be heard. It’s called a machinery murmur, as the sound increases with systole and decreases with diastole. Treatment is surgery and effective – closing the patent ductus arteriosus.
Tetralogy of Fallot
It is a right-to-left shunt, characterised by four abnormalities (hence called a tetralogy):
- Aorta originates from the right ventricle or a hole in the septum instead of the left ventricle.
- Stenosis of the pulmonary artery. Hence, deoxygenated blood from the right ventricle passed through the aorta; cyanosis (blue baby) occurs.
- Blood from the left ventricle might pass over to the right ventricle and then to the aorta.
- Enlargement of the right ventricle, as it has to do work harder by pumping more blood.
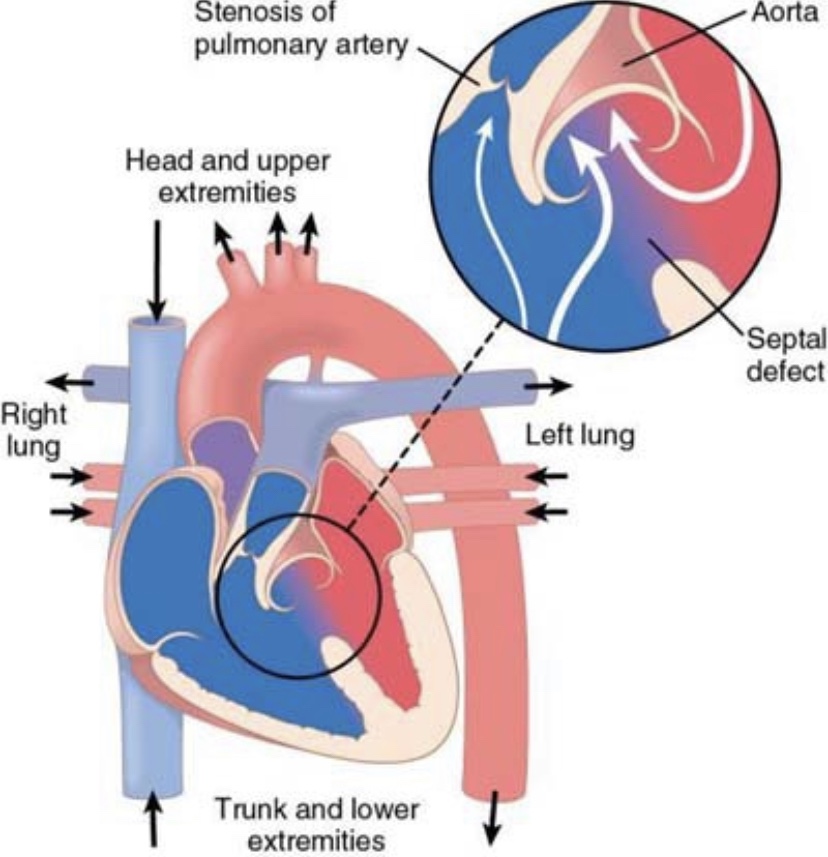

Treatment or Tetralogy of Fallot is also through surgery.
Leave a comment